- Imran Hameed
Causes of syncope are myriad and arrhythmogenic right ventricular cardiomyopathy is a rare cause of it, especially in children.
12 years old boy presented with repeated episodes of syncope at rest for 3 months. Frothing of mouth was noted in a few episodes but no aura, seizure or post syncopal weakness reported.
His BMI was 31.2 Kg/m2 and BSA was 1.2, with a HR of 95 bpm, BP 110/70, RR 14/m and was afebrile. He was mildly cyanotic and clubbed. JVP was 15 cm in sitting position with prominent A wave. Rest of the examination was unremarkable.
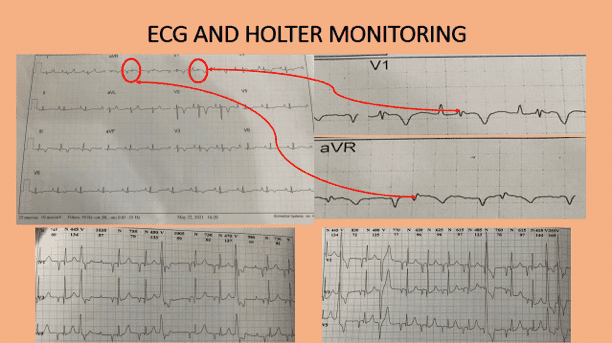
12 lead ECG showed NSR, P pulmonale, rsr’ pattern in lead V1, prolonged S wave in right precordial leads and marked T wave inversions in leads III, aVF and V1-V4. Epsilon waves were noted in leads V1 and aVR Figure 1. A 24 hours holter record showed frequent ventricular ectopics (3940/99300). No episode of VF/VT recorded however, multifocal PVCs, couplets, ventricular bigeminy and trigeminy were noted.
Transthoracic echocardiography revealed enlarged right sided chambers with RV base = 3.6 cm, mid 3.1 cm and length 6.1 cm whereas RA diameters were 4.5 and 4.4 cm. Proximal RVOT was 3.2 cm (2.67 cm/m sq.; N= < 1.9 cm sq.). Pulmonary artery main and branches were of normal caliber whereas IVC was dilated (2.3 cm) with < 50% collapse with respiration. RV free wall was highly echogenic and very thin approx. 2mm. A patent foramen ovale with Right to Left shunt was noted, see echo images. A4C RV directed view showed enlarged RV with thin and echogenic free wall with akinesia especially in basal and mid segments, see echo clips. A diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy was made.
On MRI scanning severe RV dilatation along with dys-synchronous contractions, small aneurysm formation with myocardial hyper-enhancement on Gadolinium. This feature was also noted in IVS, infero-lateral and anterolateral walls of LV showing its involvement as well. RVEDVI = 95 ml/m.sq with SV of 18 ml and RVEF of 15% only, see other clips. Thus the diagnosis of ARVC with LV involvement was confirmed. Patient was initially put on beta-blocker (bisoprolol), which didn’t showed response and then was put on amiadrone which resulted in significant improvement in symptoms. A plan for ICD placement was made but due to age and remote location of the residence of patient making follow-up difficult, parents were reluctant for the procedure.
Arrhythmogenic right ventricular cardiomyopathy affects younger males (rarely under 12 or more than 60 years) as an autosomal dominant condition with an estimated prevalence of 1:5000 in the general population. Genetic mutations involve desmoplakin, plakoglobin, and plakophilin. The disease involves desmosomes the binding units of cardiac myocytes, disruption of which results in necrosis and fibro-fatty replacement.
No symptoms, syncope, aborted cardiac arrest (mostly in adults) or sudden death (mostly in pediatric group) are presenting modes.
An international Task Force devised criteria for the diagnosis of ARVC in1994 which was updated in 20101. This includes six parameters viz, family history, ECG abnormalities, arrhythmias, tissue characteristics, echocardiography and MRI, the features of which constitute major and minor criteria. For diagnosis two major or one major and two minor or four minor criteria are needed. Of these this patient fulfilled the following major criteria:
The minor criteria noted were:
Cardiac magnetic resonance is the gold standard for diagnosis nowadays. Initially thought to be a disease of right ventricle only but lately LV involvement especially the infero-lateral wall has found to be common, thus replacing the ‘triangle of dysplasia’ with ‘quadrangle of ARVC’2. RV is more commonly involved because of its thin walls.
Arrhythmic events are the indications for treatment. In this regard beta-blockers, amiadarone and sotalol have been studied and showed beneficial results. In selected cases Calcium channel blockers have also been advocated. Heart failure is managed along the standard guidelines. Competitive sports are to be discouraged. Implantable cardioverter defibrillators are recommended to avert sudden cardiac death3. VT ablation therapy has also been recommended.
Echocardiography plays a central role in etiological delineation of syncope and is an important tool for diagnosing arrhythmogenic right ventricular cardiomyopathy.
Copyright 2023 © All Rights Reserved